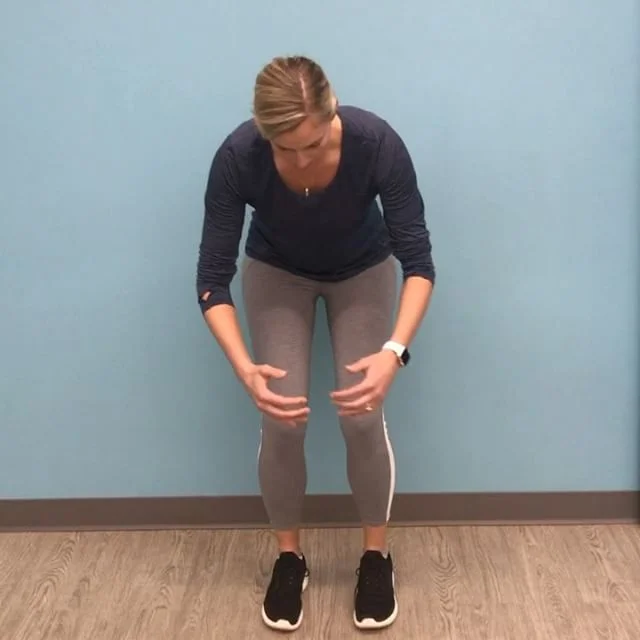
Neck and low back pain.
Rehabilitation of sporting injuries.
Recovery post surgery.
Pre-natal & post-natal pilates.
Physiotherapy / Physical Therapy
Sian Smale is an Australian-trained Musculoskeletal Physiotherapist and Clinical Pilates Instructor. As a Physiotherapist, Sian has a keen interest in helping people with neck and back pain, headaches and sporting injuries. Growing up, Sian enjoyed many sports including swimming, volleyball, field hockey and tennis. More recently yoga, cycling, and snowboarding/skiing have captivated her time.
For the past seven years, Sian has been living and practicing in San Francisco, California. Prior to moving to San Francisco, Sian worked at Physica Spinal and Physiotherapy Clinic in Melbourne, Australia. In 2009, Sian was awarded a Bachelor of Physiotherapy from La Trobe University and 2013 awarded a Masters Degree in Musculoskeletal Physiotherapy from Melbourne University. Combining her love of sport, passion for manual therapy and training in Pilates, Sian is able to design individualized treatment programs and Pilates programs that truly focus on your goals and problems.
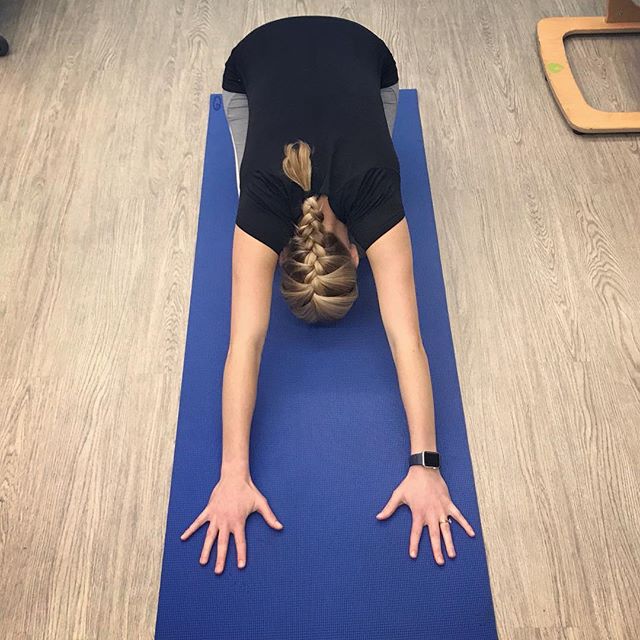
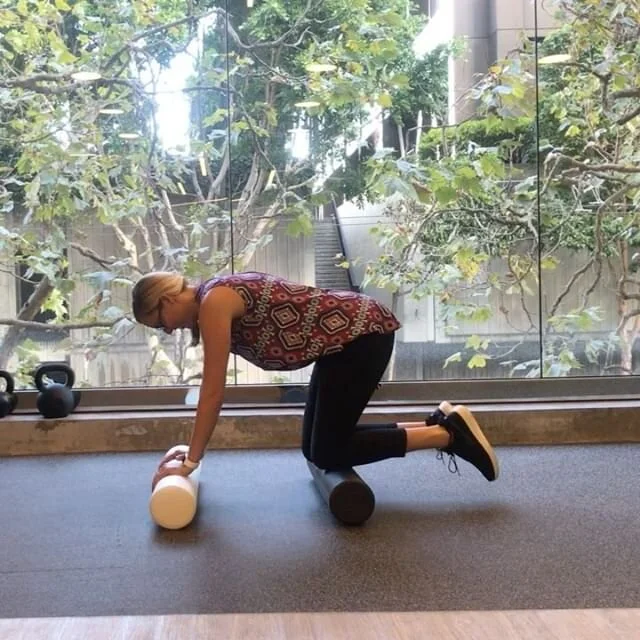
Clinical Pilates
As a Pilates instructor, Sian strives to understand herclient's goals and their problems, and to teach them the knowledge and exercises required to reach these goals. These programs can involve a wide range of equipment from pilates reformers, Redcord, fitness balls, free weights and mat work. Sian completed her clinical pilates training through DMA (Dance Medicine Australia), and is a certified Functional Movement System instructor (FMS). Sian enjoys teaching Pilates both as individual sessions and duets.
Physiotherapy Blog
Sian is a passionate blogger and founded the Physiotherapy blog Rayner & Smale in 2013. This blog contains freely available information about Physiotherapy practice. Sian enjoys reading peer-reviewed journal articles and formulating evidence-based approaches to assessment and treatment of musculoskeletal injuries. Sian's aim and passion is to continue educating Physiotherapists and health professionals world wide, share knowledge, and close the gap between science and clinical practice.
There is also a link to Sian's Wellness blog which shares information about Pilates exercises, managing your own injuries and educational material for Physiotherapy conditions. In 2016, Sian began writing guest posts for the Modern Manual Therapist.
Qualifications
Licensed Physical Therapist in California 2017-current time.
Licensed Physiotherapist and APA-titled Musculoskeletal Physiotherapist in Australia 2009-current time.
Clinical Pilates Instructor
Dry Needling Certification (Australia only) & Myofascial Decompression certification
CPR certified
APTA Clinical Instructor
Fellow of the American Academy of Orthopedic Manual Physical Therapy








.jpeg)